Recently, a team of researchers led by Bradley C Johnston of Texas A&M University (TAMU) published a heavy research result in the prestigious journal British Medical Journal (BMJ) [1].
They analyzed 40 clinical trials containing 35,548 participants and 7 major dietary regimens (low-fat, Mediterranean, very low-fat, modified fat, low-fat + low-sodium, ornish [ornish], Pritikin [Pritikin]).
They found that the Mediterranean diet was associated with a 28% lower risk of all-cause mortality, a 45% lower risk of cardiovascular death, a 35% lower risk of stroke, and a 52% lower risk of nonfatal myocardial infarction compared with minimal dietary interventions, and the low-fat diet was associated with a 16% lower risk of all-cause mortality and a 23% lower risk of nonfatal myocardial infarction. And both dietary regimens were more effective in absolute terms for high-risk patients.
As for the remaining five dietary regimens, Johnston's team found they had little or no effect.
Screenshot of the front page of the paper
Statistically, an estimated 22% of adult deaths and 15% of Disability Adjusted Life Years (DALYs) worldwide are attributed to dietary habits [2]. If this estimated figure is true, then there is no doubt that diet is a major cause of death and major diseases.
We all know that cardiovascular diseases and related deaths are the biggest killers of human health. In recent years, scientists have studied many dietary regimens in an attempt to reduce the risk of major cardiovascular events, and these dietary regimens mainly include a variety of low-fat diets, the Mediterranean diet, and diets to prevent hypertension (e.g., DASH).
Although some dietary guidelines recommend dietary regimens that may reduce the risk of major cardiovascular events, they usually rely on surrogate clinical outcomes or are based on low-quality evidence derived from nonrandomized controlled clinical studies. There have been paired meta-analyses of randomized controlled trials suggesting that some dietary regimens may reduce cardiovascular events, but the beneficial effect on mortality is uncertain [3-6].
Johnston's team noted the lack of network meta-analyses (a more precise analytical scheme) that systematically summarize randomized controlled trials and compare the effects of structured dietary regimens on mortality and major cardiovascular events such as stroke and myocardial infarction to date. Therefore, they conducted a systematic review and network meta-analysis of existing randomized controlled trials to compare the effects of various dietary regimens used to reduce mortality and major cardiovascular time.
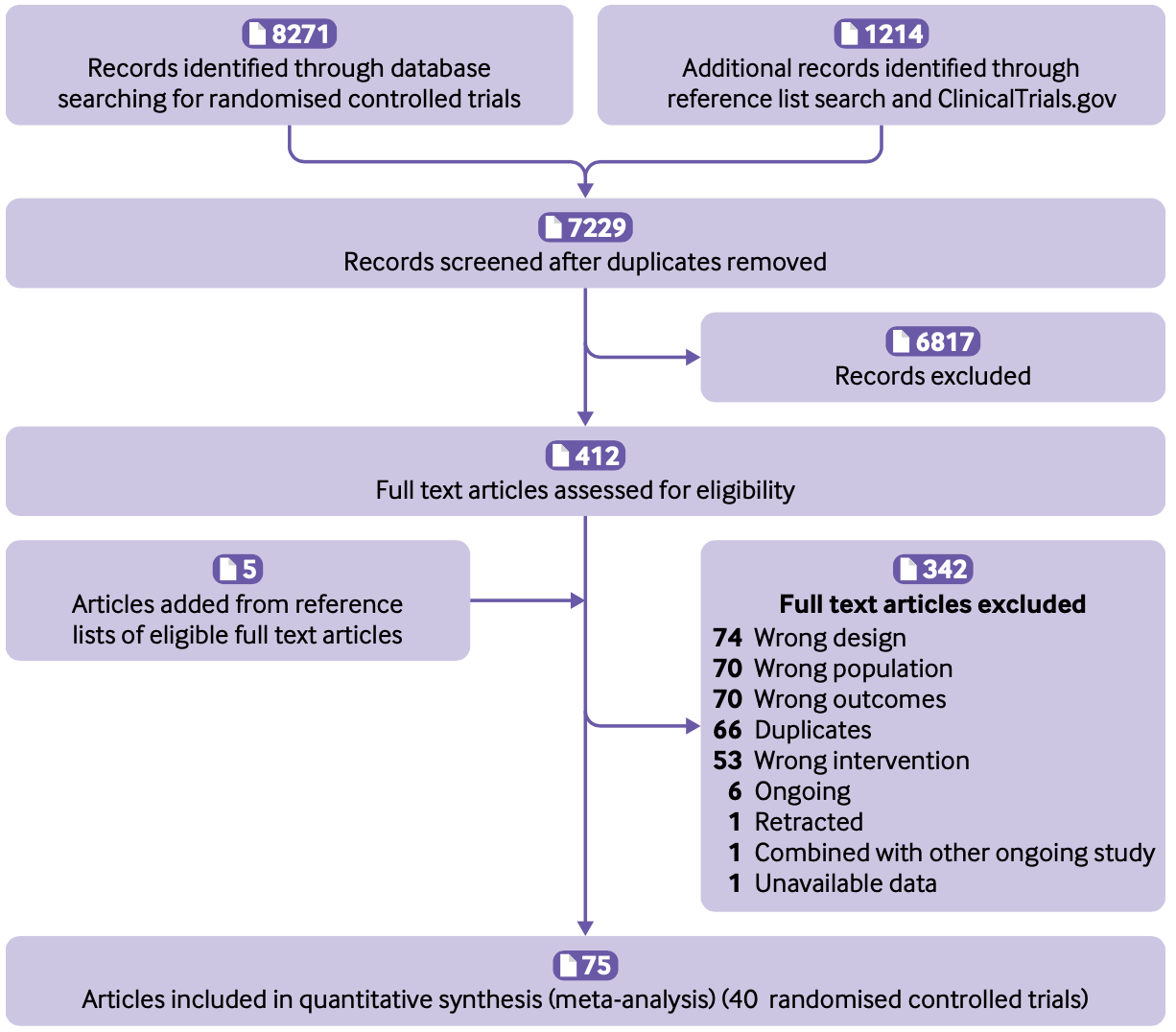
Research Process
They ultimately screened 40 randomized controlled clinical studies, involving a total of 35,548 participants, from a large number of clinical research studies.
Nine of the clinical trials (n=17632) looked at primary prevention and 31 (n=17916) looked at secondary prevention. The dietary regimens studied included: low-fat (18 studies), Mediterranean (12), very low-fat (6), modified fat (4), low-fat + low-sodium (3), Ornish (3), and Pritikin (1). The control group was a minimal dietary intervention regimen (usual clinical care) with a follow-up of 0.75-17 years.
In terms of all-cause mortality, the primary clinical outcome, the Mediterranean diet was associated with a 28% reduction in the risk of all-cause mortality and the low-fat diet was associated with a 16% reduction in the risk of all-cause mortality compared with the minimal dietary intervention. Other dietary regimens had little or no effect on mortality.
In terms of the primary clinical outcome of risk of cardiovascular death, the Mediterranean diet was associated with a 45% reduction in the risk of cardiovascular death compared with the minimal dietary intervention. No benefit in risk of cardiovascular mortality was observed with any of the other dietary regimens.
For the four secondary outcomes of angina, heart failure, peripheral vascular events, and atrial fibrillation, the Mediterranean diet was only observed to be associated with a 35% reduction in the risk of stroke, due to fewer data. This clinical benefit was not observed for other dietary regimens.
For the secondary clinical outcome of nonfatal myocardial infarction, it was also observed that the Mediterranean diet was associated with a 52% reduction in risk and the low-fat diet was associated with a 23% reduction in risk. For the last secondary clinical outcome of unplanned cardiovascular interventions, only a 43% reduction in risk was observed with the low-fat diet regimen.
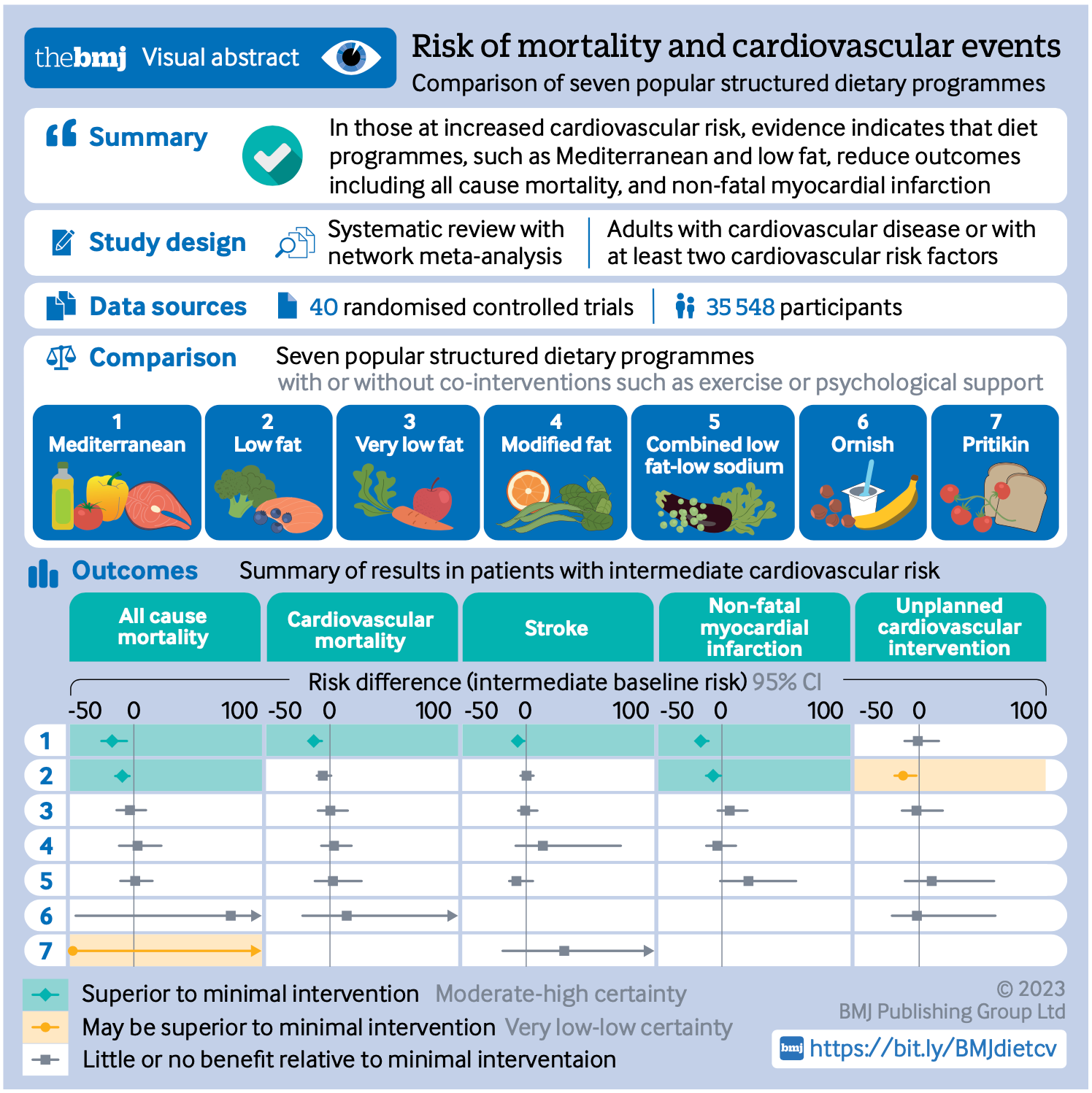
Summary chart of findings
Overall, this study by Johnston's team found that, based on moderate certainty evidence, the Mediterranean dietary regimen was superior to minimal dietary interventions for all-cause mortality, cardiovascular mortality, stroke, and nonfatal myocardial infarction; and that, based on low to moderate certainty evidence, the low-fat dietary regimen was superior to minimal dietary intervention.
There is no convincing evidence that the Mediterranean diet is superior to the low-fat dietary regimen for the prevention of all-cause mortality or nonfatal myocardial infarction when the two are compared with each other. Overall, however, the Mediterranean diet provided more benefit. As for the other dietary regimens, there is no convincing evidence that they are superior to minimal dietary interventions.
Reference:
[1].Karam G, Agarwal A, Sadeghirad B, et al. Comparison of seven popular structured dietary programmes and risk of mortality and major cardiovascular events in patients at increased cardiovascular risk: systematic review and network meta-analysis. BMJ. 2023;380:e072003. Published 2023 Mar 29. doi:10.1136/bmj-2022-072003
[2].GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393(10184):1958-1972. doi:10.1016/S0140-6736(19)30041-8
[3].Nissen SE. U.S. Dietary Guidelines: An Evidence-Free Zone. Ann Intern Med. 2016;164(8):558-559. doi:10.7326/M16-0035
[4].Ioannidis JP. Implausible results in human nutrition research. BMJ. 2013;347:f6698. Published 2013 Nov 14. doi:10.1136/bmj.f6698
[5].Ioannidis JPA. The Challenge of Reforming Nutritional Epidemiologic Research. JAMA. 2018;320(10):969-970. doi:10.1001/jama.2018.11025
[6].Zeraatkar D, Johnston BC, Guyatt G. Evidence Collection and Evaluation for the Development of Dietary Guidelines and Public Policy on Nutrition. Annu Rev Nutr. 2019;39:227-247. doi:10.1146/annurev-nutr-082018-124610



